Optimization of effects and medical costs in the system of medical care for the “heavy users” patient group
-
Copyright
© 2012 PRO MEDICINA Foundation, Published by PRO MEDICINA Foundation
User License
The journal provides published content under the terms of the Creative Commons 4.0 Attribution-International Non-Commercial Use (CC BY-NC 4.0) license.
Authors
| Name | Affiliation | |
|---|---|---|
Andrzej Ameliańczyk |
Cybernetics Department, Military Technical University, Warsaw, Poland |
|
Tomasz Ameliańczyk |
Military Institute of Aviation Medicine, Warsaw, Poland |
The paper concerns the optimization of effects and medical costs in the process of providing medical services with the Health Care System. The idea of optimization relies on the use of the opportunity to steer the demand for medical services by different segments of potential patients. For this purpose the most important patient groups were identified from the perspective of effects and medical costs. A special attention was paid to the groups of patients of the HEAVY USERS (HU) and the LIGHTHEARTED USERS (LU) types – the so called „carefree” patients. The paper contains the concept of the method identifying HU type and LU types patients. Patients of these groups generate relatively high medical costs. The costs are usually unjustified (the losses of the HCS) additionally leading to the decrease of medical and social effects of medical care. Identification and classification of the groups of patients further enables the use of the application of adequately selected clinical paths and the medical intervention system.
Introduction
Constant medical progress and related ever higher costs are generated by the application of ever more novel and more effective diagnostics and therapeutic methods, changes in the age structure of the population (the extension of average life expectancy) or higher expectations of the patients’ life quality cause constant pressure to increase expenditure on the health care system (HCS). On the other hand limited financial resources of public payers result in the situation in which there are no worldwide public HCSs which are able to satisfy health care needs of their all citizens to the full extent. In the light of this, the optimum redistribution of the available resources of the HCS to be used in the best possible manner is becoming a burning issue. One of the sources of generating high costs in the HCS what is indicated in ever more numerous scientific papers is the population of patients described as heavy users. This is a heterogeneous group of patients whose common attribute is the consumption of significant resources of the HCS. Among them one can distinguish persons who in case of a serious disease tend to, usually periodically, increase the demand for the HCS resources (so called N type heavy users) and persons for whom there is no justified, from the medical perspective, need to frequently use the system resources (H type heavy users).
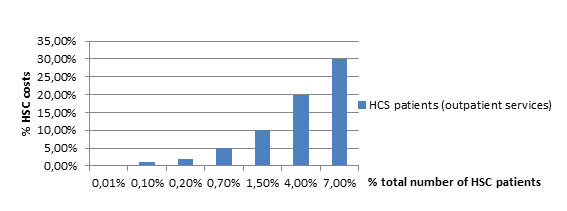
The scale of the phenomenon is not precisely known. In the worldwide publications in which the phenomenon of occurrence of the heavy user patients was examined taking into account the example of Emergency Departments (ED) show that the population may constitute between 0,2% and 11% of patients using the services of ED at the same time generating between 1,9% and 32% of all visits. The problem of heavy user patients in Poland is still less well-known however ever more interest in the phenomenon is being observed. The analyses conducted in the companies offering private outpatient medical care in Poland at the same time clearly point out the existence of the said group of patients – the group of 1,5% most expensive patients generated 10% of medical costs (and 4% of patients generate 20% of medical costs respectively):
pacjenci SOZ (usługi ambulatoryjne – HCS patients (outpatient services)
The aim of the analysis is the attempt to identify the patient group of so called heavy users, identification of common and differentiating attributes of the selected subgroups (H and N types of heavy users). Limited resources of each and every HCS, including the financial ones, require the rationalization of the health care expenses borne.
One of the ways of achieving the goal is the optimization of the clinical paths management proposed to individual identified patient groups included in heavy users type. To identify heavy user patients the author’s survey model was developed aiming at the analysis of the identified subgroups of heavy users (N and H types) which is based on broadly understood algorithms of the pattern identification [1,12]. To achieve it so called the living space, disease patters, health patterns and patters of respective subgroups of heavy users were identified.
The group of patients described as heavy users is not homogeneous. Among them two main subgroups may be distinguished:
N type heavy users – patients who in case of being affected by a serious disease (usually periodically) increase the demand for the HCS resources. After some time the manner of using the HCS resources usually returns to the level from before the disease or remains at a higher level. This group entails patients with chronic diseases. Due to similar behavior patterns the patient group is periodically included in the N type heavy users.
H type heavy users – persons who do not seem to have a justified, from the medical perspective, need for frequent use of the HCS resources. In this group of patients the vast majority is constituted of persons with psychosocial problems with frequent co-morbidity of chronic diseases [6]. Periodical increased use of the HCS resources is observed with the patients. In case of the constantly increased use of the HCS resources the behavior pattern of the patients is similar to patients with chronic diseases.
The division of heavy user (N and H types) patients is not entirely unequivocal (dichotomous) due to the possibility of the occurrence of mixed situations particularly in the group of patients characteristic for H type heavy users. The survey results indicated that for the heavy users group certain characteristic attributes may be distinguished as common e.g. in case of frequent seeking help in Emergency Departments was observed that previous number of visits, previous psychiatric treatment, being lonely and the feeling of loneliness predisposes to remain a heavy user [7]. Another characteristic which is noticed by the researchers in Poland and which is aimed at helping to identify heavy user patients is the observation of a big number of different diagnoses (according to ICD-10) assigned to individual patients.
In case of some patients using private outpatient care in Poland the number of diagnoses according to ICD-10 has amounted to dozens within the last 12 months. In the population of the patients ca 1,5-2,0% of them uses medical consultations at least 26 times per year i.e. every two weeks on average. Among patients covered by private outpatient care in Poland almost 6% of diagnoses are Z00 and Z01 according to ICD-10 (General examination without any diseases and the diagnosis of a disease and another special examination without any ailment and the diagnosis of the disease respectively). The analysis of the available data allows to point premises enabling identifying heavy user patients.
Table 1. Characteristics of H and N type heavy users
| Characteristic attributes | H type heavy user | N type heavy user |
| Frequency of using HCS resources | high | |
| Effectiveness of using HCS resources | usually low | |
| Time of demand for increased HCS resources | usually long, periodic | usually shorter, irregular |
| Diagnosis of disorder | usually psychosocialless frequently organic | usually organic |
| General health / additional medical examination | within the normal range | usually some irregularities are found |
| Occurrence of significant disease risks | average at most | increased |
| Number of diagnoses according to ICD-10 | usually high | low |
| Number of specialist consultations within the last 12 months | usually high | close to the average in the population |
The occurrence of the above mentioned characteristic attributes allows only for preliminary diagnosis in the context of identifying heavy users of individual types. The division does not have to be, as mentioned above, entirely dichotomous. „Mixed cases” combining those two types are possible. A mixed case is a special H type heavy user case. It requires special approach in proposing further treatment. The initial characteristic of heavy users may be summed up as follows:
Heavy users N type (HU N type)
Due to inter alia complex health issues and the way of the organization of delivering health care the patients as a rule use health care resources intensively for some time with no satisfying effects for them in a short time. In the period the description of their behavior is the reflection of the behavior of the so called „classic” heavy user (H type). After some time in this group of patients, contrary to H type heavy users, return to behavior typical for the period preceding the health care problem or permanent increase of the demand for medical care services (the diagnosis of a chronic disease) is observed. The health needs of patients have been met (the disorder has been property diagnosed and proper treatment has been introduced) or after some time they have realized that the health care system is not capable of coping with their health problems (the attitude of resignation).
H type heavy users (HU H type)
This group of patients intensively uses medical care, most frequently in the aspect of a few diseases in a significantly longer period of time (the so called regular patient). These patients require an entirely different path of treatment. The characteristic attribute of the patient group is relatively good health most often confirmed by correct (within the normal range) results of additional examinations. On the whole physicians easily recognize such attitudes. There is a certain danger of the risk of overlooking a disease due to the reduced alertness of a physician to an ailment reported by a patient.
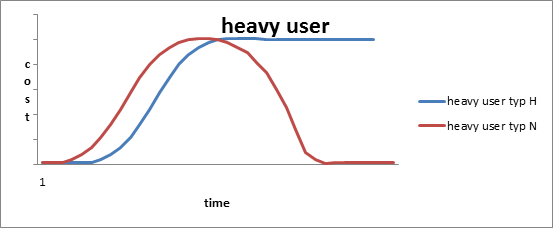
A strict division between heavy users of H type and N type is difficult to draw and burdened with a significant risk of a medical error (in particular the so called mixed case). Clear diagnosis is frequently difficult what causes the process of medical care (including treatment) to be significantly prolonged. It is detrimental both in case of N and H types. In the range of large populations of patients covered by HCS care the phenomenon poses a significant health, economic and social problem. Designing a tool to guarantee a proper diagnosis would be a big opportunity to effectively treat both groups of patients and secondly to efficiently distribute public resources for medical care. The social dimension to shorten the time to remain a HU (shortening the time of the societal exclusion due to the disease) is of the essence as well. In Figure 2. typical characteristics of costs for both HU types are presented.
In the first phase of observation both patient groups are difficult to differentiate solely based on this characteristic. After a certain time an „observable difference” appears which may be a premise for the final finding. The two above mentioned patient groups generate relatively high social treatment costs. While the fact is fully justified in the case of N type heavy users inasmuch additional costs generated by H type heavy users are not justified. A significant group of HU H type in the overall patient population may limit the access to medical services of other patients to a considerable extent. Precise identification and classification of the patient groups to propose optimum clinical paths is a critical problem. The process may be realized based on definitions of respective classification attributes of individual patient groups having the aspect of measurability. The process is a typical process of detection of individual elements of the fixed population.
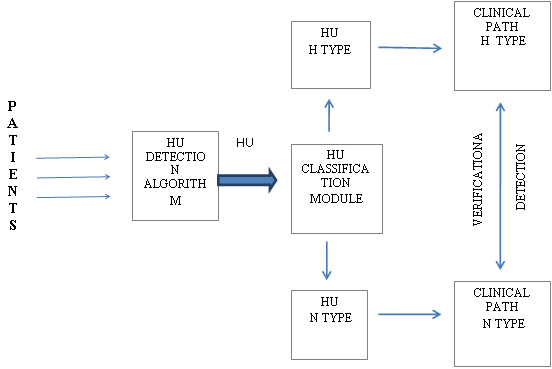
Detection of heavy users – the diagnostic process allowing to precisely detect the group of patients complying with the criteria of the heavy users definition. The scheme of the detections presented in Figure 3.
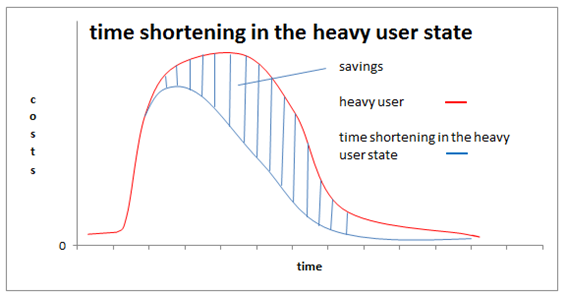
Depending on the period of the patients „existing” in the „state of heavy users” disproportionately high costs connected with ineffective functioning of the health care system are generated. Shortening the time of the patients existing in the heavy users state through the recommendation of specific and adequate as well as more effective way approaching the correct diagnosis and treatment to them should give in effect the decrease of costs related to the functioning of the health care system as a whole:
To achieve this goal, it is essential to identify patients out of the population covered with the health care of the patients whose profile corresponds to a patient falling into the heavy users category. Initial designation of the patients may rely on the analysis of parameters of the cost curve. A more effective and precise method is the identification of those patients with pattern recognition algorithms [1,3,12]. It is required to define health patterns, diseases patterns and patterns of N and H type heavy users respectively in the so called life space [12]. Such an approach offers a very helpful support of the diagnostic process based on the results of additional examinations enabling the construction of merit indicators [4]. The idea of identification algorithms and the classification of heavy users is to define objective, complex indicator of a patient’s state of health understood as property defined „distance” from the pattern of a patient’s health with respect to a corresponding sex and age group and some characteristic of the closest disease threat [1,2,3,4,12]. These two characteristics, except for the very simple characteristic illustrating the intensity (costliness) of the use of HCS resources allow for the creation of the so called space of identification which enables to identify potential N and H types of HU [4]. In this space the sought patterns of N and H type HU are easy to be built. Each patient, on the basis of their features on the medical examination results is possible to be placed in the space setting respective merit indicators [4]. Having a sufficient patient data base („treatment history”) one can precisely calibrate the said model describing the sought threshold values of the necessary indicators. This can be done though a computer simulation with the use of patient data base and experts’ findings. After the detection stage is carried out and then the classification of respective subgroups of heavy users, the patient will be offered a individualized clinical path, which in case of N type heavy users will be aimed at proper diagnosis in the shortest possible time. The matter which requires an in-depth analysis, with the involvement of experts from various fields including ethics is the manner of further procedure towards H type heavy user patients. These patients have to be covered with a dedicated program with the emphasis on frequent non-somatic disorders. It appears essential to work out a socially acceptable strategy of cost reduction for the treatment of the population of the patients including special medical and organizational procedures. Introduction of the detection system and further classification of heavy user type patients should cause the obtainment of medical, social and economic benefits. Medical benefits encompass faster accurate diagnosis in case of N type heavy user patients, coverage with the dedicated care program for H type heavy user patients to a big extent aimed at frequent occurrence of psychosocial problems arising in the group. The implementation of the system is justified from the social and economic perspectives. In the longer time horizon it should result in more rational utilization of HCS resources what should be reflected in the availability of HCS resources to a bigger patient group. Not without significance is the optimization of expenditure incurred for HCS. A separate and very important issue from the perspective of the optimization of global patient treatment costs and economic and social effects of health care is so called “the light-hearted patient” issue.
Light-hearted patientis a patient who temporarily (frequently in a very long time) does not generate any health care costs. This group encompasses patients who chronically (due to different reasons) avoid contacts with health care.
This group is not homogeneous either. Patients of the group sooner or later generate very high treatment and social costs connected with the too-late diagnosis of a disease. The problem of detection and classification of this patient group arises. The issue of “light-hearted user” patient type is as important as the issue of “heavy user” patient type. The joint solution of this complex issue may lead to substantial effects of the optimization of HCS activity. The key issue is the problem of heavy user patient type the solution of which creates an opportunity to significantly decrease the number of light-hearted patients with the same capacity of HCS budget. A simplified model of the detection space and the classification of patients-users of HCS is presented below. The model presents the opportunity to detect previously discussed patient class and adjust proper strategies of medical treatment (proper clinical paths or other medical interventions).
Mathematical detection space model
A simplified model of the detection process and classification of patient population is presented below. X symbol stands for a class (population) of patients identified with the variable x ε X (x – patient identification number e.g. PESEL). The X class de facto is the patient database and x ε X is a respective e-health x patient record. On the basis of data contained in the X base any models describing the patient’s health (life spaces), health threat, disease detection, diagnostic, clinical paths, special attribute patient group detection spaces, etc. may be built [1,4,5,12]. To optimize the functioning of the HCS, a model of detection model of the patient group significant in the area of costs and treatment effects will be presented. The detection (and then classification) the x ε X patient requires the definition of respective qualification attributes which are important
from the perspective of the classification aim. The attributes may be in particular:
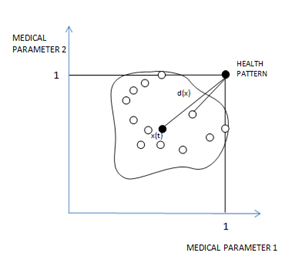
- general indicator of the patient’s health d(x) [1,12]
- indicator of the resources (costs) consumption HCS n(x) [3]
- indicator of the present disease threat to a patient g(x) [1]
- indicator of range of patient treatment h(x)
In more precise models there is a possibility to define many more other qualification attributes. The indicator of the patient’s general health pattern is generally understood as “distance” of the patient’s health from the pattern of a patient’s health (for a specified age and sex of the patient) [1]. The indicator of the HCS resources consumption may be defined as a number of medical consultations (examinations) in a specified time unit or directly as a cost [5]. The indicators of the disease threat are defined by analogy as the distance of the patient’s health from the patterns of respective disease units [12]. The indicator of the range of patient’s treatment is generally defined as the quotient of number of different specialists visited in a time unit against the total number of medical consultations.
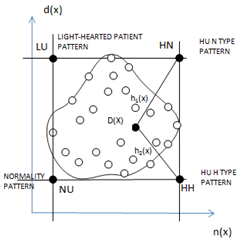
In Figures 5 and 6 the simplest cases of the so called life space are presented and the detection space covering only two attributes due to presentation reasons [1,12]. The detection space D(X) presented in Figure 6. is a class of “pictures” of x X patients in terms of classification attributes adopted in the model. Defining respective relationships of the patient’s health specificity (such as: ‘normality”, “light-heartedness”, H type “nuisance”, N type “nuisance” as Pareto relations it is easy to define patterns: normality, light-heartedness, H type and N type “nuisances” as so called an end to the class D(X) [12]. These are respectively marked in Figure 6. points: HH, HN, LU, NU. They may be interpreted as pictures of virtual, standard patients of respective classes.
Introduced relations allow for additional comparison of pictures of patients in different aspects as well as for definition classes of patients of particularly important attributes in the optimization process such as: the class of “the most hypochondriac” patients, the class of patients where there are no other as hypochondriac as them, the class of patients where there are no other as light-heartened as them in the population etc [1,12]. The D(X) space enables defining and examining many other distance characteristics very valuable for the detection and classification of respective patient groups in Figure 6. exemplary distances of the picture of a selected x patient from HU N type pattern and from HU H type were marked.
Conclusions
Extremely high rate of information technology of the medical care offers an enormous opportunity to build the so called Computer Systems of Medical Decisions Support. Patient data bases created in many countries (based on so called e-health records and computer-interpretable clinical paths enable complex optimization of medical care management processes in particular the support of the medical diagnostics and treatment processes [1,12]. These systems allow for an enormous opportunity of rationalization (optimization) of the structure of the demand for medical services through the possibility of detection (identification) of individual classes of HCS users and later the opportunity to adjust corresponding clinical paths to the specificity of the groups. The presented version of space detection model simplified for the purpose of the limited space in this work may be a very useful tool of versatile analysis of the medical services consumption structure offered by HCS primarily a tool of support to optimization of medical care processes. The model after corresponding calibration and simulations will allow to designate corresponding patient groups for optimal medical care through offering properly designed clinical paths for these patient groups and the system of proper medical intervention as well as organizational and legal processes of health prevention as well as global health policy making. The following step may be the construction of patients’ behavior simulator based on the presented model of the space detection which would allow for examination (and optimization) of the effects of health policy implemented at different levels of management.