Assessment of quality of life in patients with schizophrenia and their caregivers in selected Central and Eastern European countries: A literature review
-
Copyright
© 2015 PRO MEDICINA Foundation, Published by PRO MEDICINA Foundation
User License
The journal provides published content under the terms of the Creative Commons 4.0 Attribution-International Non-Commercial Use (CC BY-NC 4.0) license.
Authors
Background: To investigate the impact of schizophrenia on quality of life (QoL) of patients and caregivers in seven CEE countries, by conducting a literature search.
Methods: Search was performed in publicly available databases to identify publications from 1995 to 2012 related to schizophrenia and QoL. Publications included those describing health-related QoL data of negative symptoms in patients with schizophrenia.
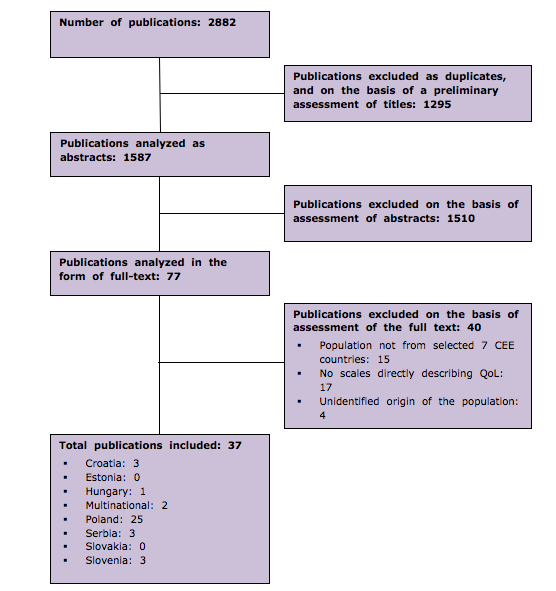
Results: Out of an initial search of 2882 abstracts, 1587 were excluded based on duplication or preliminary screening of titles, and a further 1550 publications were excluded based on screening of the abstracts (1510) or full-texts (40). Thus, 37 primary publications related to QoL of patients with schizophrenia and caregivers were identified. Due to differences observed in the identified studies, it was not possible to make direct comparisons nor to pool data for analysis. However, it was consistently reported that schizophrenia greatly affected the QoL of patients and had a significant negative impact on the QoL of caregivers, such that their QoL was considered similar to the patients themselves. In addition, patients with schizophrenia experienced significant stigmatization and discrimination. In general, the presence of negative symptoms was not well-documented in the literature and available antipsychotics had limited impact on the treatment of negative symptoms.
Conclusion: Schizophrenia significantly reduces QoL of patients and their caregivers. Further research is needed to better understand the drivers of impaired QoL caused by schizophrenia, in particular the negative symptoms of schizophrenia, and how best the burden of illness and associated stigmatization and discrimination may be reduced.Introduction
Schizophrenia is one of the most common psychiatric disorders, affecting approximately 1% of the world’s population [36] and is a leading cause of disability [48]. Lifetime prevalence of schizophrenia is high, ranging from 0.4 to 1.4%, due to the early age of onset and chronic course of the disease [36].
The impact schizophrenia upon quality of life (QoL) has been an active area of research for many years. Schizophrenia is ranked among the op ten leading causes of disease-related disability in the world and has consistently demonstrated a major negative impact on QoL [48]. The chronic nature of schizophrenia particularly affects the social dimension of QoL. Decreased cognitive and social skills, and hypersensitivity to criticism and stress, can lead to patients becoming isolated from society and the object of stigmatization [35]. Therefore, treatment goals for patients with schizophrenia not only include reducing the frequency, duration and severity of episodes and overall morbidity, but also improving psychosocial functioning and QoL [34].
Assessment of QoL can provide an additional measure of treatment outcome for patients with schizophrenia. In recent years, a large number of scales have been developed to determine well-being and QoL in patients with schizophrenia [35]. Many individuals with schizophrenia rely on informal daily care, which is typically undertaken by family members, most often parents or siblings [2]. For family members who are caregivers, schizophrenia poses numerous challenges, including management of the patient’s illness and adjustment to the negative impact on the patient’s daily functioning.
1. Objective
The aim of the study was to identify available information about the impact of schizophrenia, and particularly the negative symptoms of schizophrenia, on QoL in patients and caregivers across seven Central and Eastern European (CEE) countries. In addition, data on stigmatization and discrimination in patients with schizophrenia was obtained.
Methods
A literature search was performed in seven CEE countries (Croatia, Estonia, Hungary, Poland, Serbia, Slovakia and Slovenia). The search strategy for MEDLINE via PubMed, Cochrane Library and Centre for Review and Dissemination databases was developed using the term ‘schizophrenia’ and its synonyms. A targeted search was performed using specific filters to identify:
- publications from key countries: the country name was combined with the schizophrenia synonyms search strategy
- relevant papers on the negative symptoms of schizophrenia: the term ‘negative symptoms’ and its synonyms were added as a filter
- publications concerning QoL: terms including ‘health ‘quality of life’ and scale names (for example, ‘EQ5D’ or the European Quality of Life Scale [EuroQOL]) were added as a filter (this search was conducted only in MEDLINE via PubMed)
- publications concerning burden of schizophrenia: filters including ‘stigmatization’, ‘discrimination’, ‘costs’ and ‘burden of disease’ were used (this search was conducted in all databases).
In addition to a general search of publicly available databases, a search was conducted locally in each of the participating countries to include publications in local languages. The searched sources of data were: the local HTA agency databases, local patients registries, national medical journals, databases of national health services, national/central statistical office, national psychiatric association and other relevant sources (e.g. PhD thesis).
The search consisted of publications from 1995 to 2012 (primary studies, reviews and systematic reviews) on the QoL, stigmatization and discrimination of patients with schizophrenia (F20 in the International Classification of Diseases − Version 10 [ICD-10]). All publications that included QoL results were analyzed in relation to assessment of negative symptoms.
Results
1. Quality of life
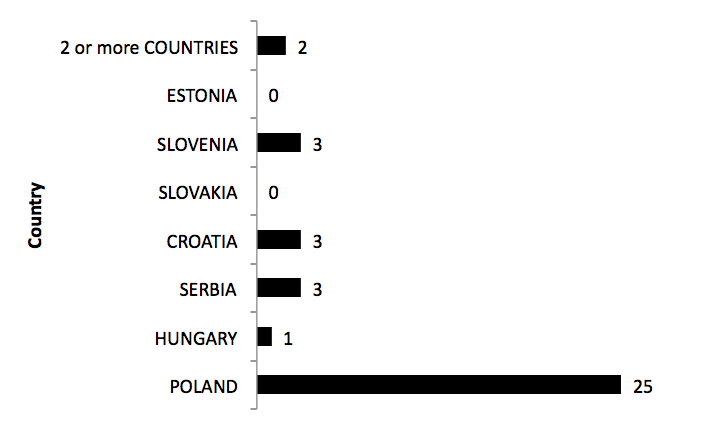
Out of an initial search of 2882 abstracts, 1295 were excluded based on duplication or preliminary screening of titles and a further 1550 publications were excluded during screening of the abstracts (1510) or full texts (40). The remaining thirty-seven primary publications from the seven CEE countries were included in the analysis (Figure 1; a PRISMA flowchart is provided in the appendix).
Thirty-five of the studies were based in one country only and two were multinational European studies: StoRMi [12] (involved 22 countries including Croatia, Estonia, Poland, Slovakia and Slovenia) and EDEN [43] (based on five countries including Poland and Slovakia). A detailed list of all studies is presented in Table 1.
Table 1. List of studies included in the analysis
| Publication | Country | Instrument(s) | Number of timepoints of QoL measurement* | Group evaluated** |
| Adamowski et al. 2009 [1] | Poland | Specific (MANSA) | 3 | Patients (F20-F29): inpatients vs day-care ward |
| Cechnicki et al. 2007 [5] | Poland | Specific (QoLI) | 1 | Patients (F20) |
| Chądzyńska et al. 2002 [7] | Poland | Specific (Mercier and Tempier Scale) | 1 | Patients vs family members |
| Chądzyńska et al. 2003 [8] | Poland | Specific (Mercier and Tempier Scale) | 1 | Patients vs family members |
| Czernikiewicz & Górecka 2003 [10] | Poland | Specific (QLS, SQLS) | 1 | Patients (F20) |
| Czernikiewicz et al. 2005 [11] | Poland | Specific (QLS) | 1 | Patients (F20) |
| De Marinis et al. 2007 [12] | 22 countries (including Croatia, Estonia, Poland, Slovakia, Slovenia) | Generic (SF-36) | 3 | Patients (F20 or other psychotic disorder): conventional oral antipsychotic vs conventional depot antipsychotic before switching to long acting risperidone |
| Dernovsek et al. 2001[13] | Slovenia | Specific + Generic (QLS, EQ-5D) | 1 | Patients (F20) |
| Główczak et al. 1997 [14] | Poland | Specific (Mercier and Tempier Scale) | 1 | Patients (F20) |
| Golubovic et al. 2010 [15] | Serbia | Specific (QLS) | 8 | Patients (F20 or schizoaffective disorders) treated with: atypical antipsychotics vs classical antipsychotics |
| Górecka & Czernikiewicz 2004 [16] | Poland | Specific (QLS) | 1 | Patients (F20) |
| Górna et al. 2005 [17] | Poland | Specific + Generic (SFS, WHOQOL- BREF) | 2 | Patients (F20) vs healthy subjects |
| Górna et al. 2007 [19] | Poland | Specific + Generic (SFS, WHOQOL- BREF) | 1 | Patients (F20): with depression vs without depression |
| Górna et al. 2008 [18] | Poland | Specific + Generic (SFS, WHOQOL- BREF) | 3 | Patients (F20) |
| Hanuszkiewicz et al. 2007 [20] | Poland | Specific (LQoLP) | 1 | Patients (F20) |
| Jaracz et al. 2008 [22] | Poland | Specific (SFS) | 3 | Patients (F20) |
| Jarema et al. 1995 [25] | Poland | Generic (SF-36) | 2 | Patients (F20 or depression): inpatients vs day-hospital vs rehabilitation unit |
| Jarema et al. 1997 [24] | Poland | Generic (SF-36) | 1 | Patients (F20): inpatients vs patients from day-hospital vs patients from day-care centre |
| Jarema & Konieczyńska 2000 [23] | Poland | Generic (SF-36) | 2 | Patients (F20) (men vs women) |
| Jarema et al. 2002 [26] | Poland | Generic (SF-36) | 2 | Patients (F20) (men vs women) |
| Jukić et al. 2003 [27] | Croatia | Specific (QLS) | 1 | Patients (F20) treated with: conventional antipsychotics vs novel antipsychotics |
| Kasperek et al. 2002 [28] | Poland | Specific (QoLQ) | 2 | Patients (F20) from: social skills training group vs psychoeducation group |
| Konarzewska et al. 2012 [29] | Poland | Specific (QLS) | 1 | Patients (F20 vs F20 addicted to alcohol) |
| Konieczyńska et al. 1997 [30] | Poland | Generic (SF-36) | 3 | Patients (F20) |
| Margetić et al. 2011 [31] | Croatia | Generic (Q-LES-Q-SF) | 1 | Patients (F20) vs relatives (key caregivers) vs healthy people |
| Mihajlović et al. 2011 [35] | Serbia | Specific + Generic (SFS, SWLS, WHOQOL-BREF) | 1 | Patients (F20) treated with: haloperidol depot vs risperidone long-acting |
| Opalić & Femić 2008 [37] | Serbia | Specific (combination of LQoLP and MANSA) | 1 | Patients (F20) vs healthy controls |
| Pąchalska et al. 2001 [38] | Poland | Specific (QLS) | 1 | Patients (F20) vs patients incurred a closed-head injury |
| Pentek et al. 2012 [45] | Hungary | Generic (EQ-5D) | 1 | Patients (F20) vs general population |
| Pesek et al. 2010 [41] | Slovenia | Generic (WHOQOL- BREF) | 1 | Patients (F20) |
| Pesek et al. 2011 [40] | Slovenia | Generic (WHOQOL- BREF) | 1 | Patients (F20) |
| Popławska et al. 2004 [42] | Poland | Specific (IMHC 2000) | 2 | Patients (F20 or depression) treated with: pharmacology and psychoeducation vs pharmacology |
| Priebe et al. 2011 [43] | 5 countries (including Poland and Slovakia) | Specific (MANSA) | 4 | Patients (F20-F29, F30-F39, F40-F49) |
| Ružić et al. 2008 [45] | Croatia | Generic (Q-LES-Q) | 1 | Patients (F20-F29) who committed the crime of murder or attempted murder in state of insanity |
| Spiridonow et al. 1998 [46] | Poland | Specific (Mercier and Tempier Scale) | 1 | Patients (F20) vs healthy controls |
| Tomczak 2005 [50] | Poland | Generic (WHOQOL- BREF) | 1 | Patients (F20) vs healthy controls |
| Tomczak 2006 [49] | Poland | Generic (WHOQOL- BREF) | 1 | Patients (F20) vs healthy controls |
*QoL could be evaluated once (at a specific time) or two or more assessments of QoL were carried out in different time period
**F20 = Schizophrenia (according to ICD-10)
MANSA=Manchester Short Assessment of Quality of Life Scale; QoLI=Quality of Life Inventory; QLS=Quality of Life Scale; SQLS=Schizophrenia Quality of Life Scale; SF-36=Short Form (36)n Health Survey; EQ-5D=Euro Quality of Life 5-Dimension Scale; SFS=Social Functioning Scale; WHOQOL-BREF=World Health Organization Quality of Life Brief Instrument; LQoLP=Lancashire Quality of Life Profile; QoLQ=Quality of Life Questionnaire; Q-LES-Q-SF=Quality of Life Enjoyment and Satisfaction Questionnaire – Short Form; SWLS=Satisfaction with Life Scale.
We analyzed publications in terms of the number of estimates of QoL (time points), populations in which QoL was assessed and instruments used to evaluate QoL.
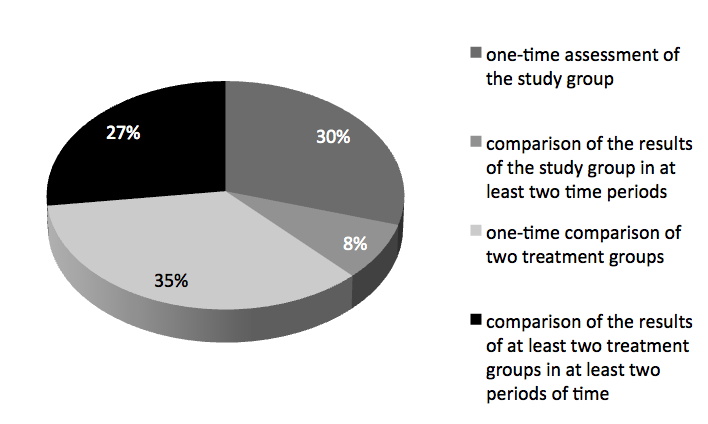
Four types of study design were observed, relating to study time-length and relationship factors (Figure 2). In the simplest approach the QoL of the analyzed group was evaluated once (at a specific time-point). In a more complex approach, two or assessments of QoL carried out at baseline and other pre-specified time-points were compared. Other studies compared the QoL in two or more groups of individuals, either at one time-point or at two or more time-points. The percentage distribution of the various types of studies is presented in Figure 2.
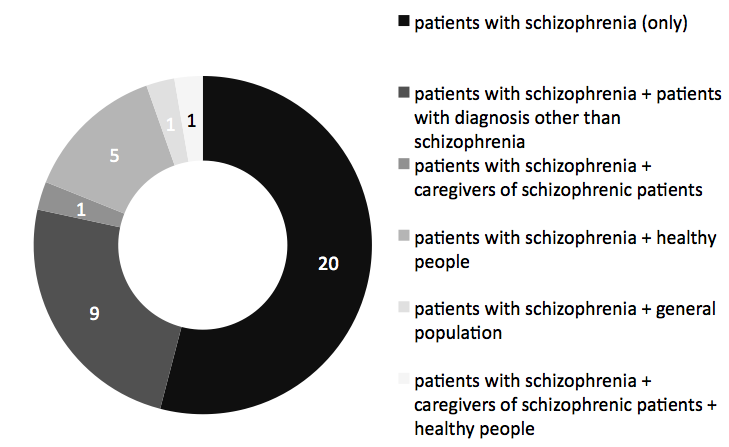
The evaluation of patients’ QoL was carried out most often by themselves (self-evaluation). However, in some studies, the assessment was made by healthcare professionals (doctors, nurses), caregivers or relatives. In 46% of the studies, QoL of other groups was also assessed, such as patients with mental disorders other than schizophrenia, caregivers of patients with schizophrenia, healthy people (trial sample) or a sample of age- and country-matched population (Figure 3).
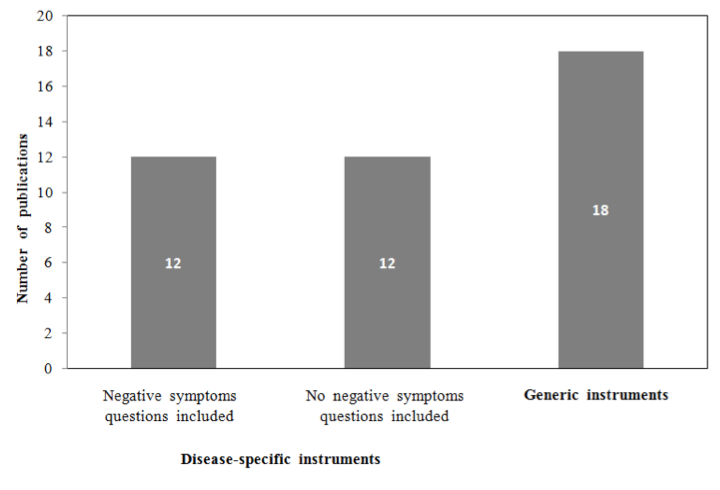
Schizophrenia was found to greatly affect the QoL of patients and had a significant negative impact on the QoL of caregivers. Both general QoL questionnaires and those specific for schizophrenia were reported. However, only a few instruments addressed the impact of negative symptoms on QoL (Figure 4).
Questionnaires not specific for schizophrenia were as follows (a detailed list of studies and instruments are presented in Table 1):
- EQ-5D: includes domains such as Mobility, Self-Care, Usual Activities, Pain/Discomfort And Anxiety/Depression
- Quality of Life Enjoyment and Satisfaction Questionnaire-Short Form (QLESQ-SF): measures satisfaction with domains such as physical health, mood, work and household activities on a 5-point scale
- 7-point Satisfaction with Life Scale (SWLS)
- Short Form-36 (SF-36) questionnaire: includes domains such as Vitality, Physical Functioning, Bodily Pain, General Health Perceptions, Physical Role Functioning, Emotional Role Functioning, Social Role Functioning and Mental Health
- World Health Organization Quality of Life Instrument – BREF (WHOQOL-BREF): includes domains for Overall QoL and General Health, Physical Health, Psychological Status, Social Relationships and Environment
- Quality of Life Questionnaire: includes domains for General Well-Being, Interpersonal Relations, Organizational Activity, Occupational Activity, and Leisure and Recreational Activity.
The disease-specific questionnaires used in assessment of QoL of patients with schizophrenia were as follows (a detailed list of studies and instruments are presented in Table 1):
- Lancashire Quality of Life Profile (LQoLP): an interviewer-administered instrument for patients with chronic mental illness
- Manchester Short Assessment of Quality of Life (MANSA): a questionnaire for patients with severe mental illness (includes some questions about satisfaction with leisure activities and the quality of social relationships based on a 7-point satisfaction scale)
- Quality of Life Interview (QoLI): an instrument dedicated to patients with mental illness
- Heinrichs Quality of Life Scale (QLS): schizophrenia-specific QoL instrument featuring a 21-item scale
- Schizophrenia Quality of Life Scale (SQLS): a brief self-report measure
- Social Functioning Scale (SFS): an instrument developed and validated on outpatients and conducted as a verbal interview.
Three other questionnaires less commonly presented in publications were also identified: the Liebermans’ Quality of Life Questionnaire (QLQ), Mercier and Tempier Scale and IMHC 2000 (see Table 1). Only a few of the disease-specific QoL instruments measured dimensions relating to negative symptoms, as listed below:
- Lancashire Quality of Life Profile (LQoLP): an extensive interviewer-administered instrument for patients with chronic mental illness including schizophrenia, offering objective QoL indicators and subjective QoL estimates. in addition, the LQoLP assesses positive and negative affect, positive and negative self-esteem and global well-being
- Heinrichs Quality of Life Scale (QLS): a 21-item scale for patients with schizophrenia based on a semi-structured interview designed to assess deficit symptoms over the preceding 4 weeks. The items are grouped into categories: Intrapsychic Foundations, Instrumental Role and Common Objects and Activities
- Schizophrenia Quality of Life Scale (SQLS): a 30-item self-report questionnaire designed for patients with schizophrenia, consisting of three scales (Psychosocial, Motivation and energy, and Symptoms and side-effects)
- Social Functioning Scale (SFS): a 79-item questionnaire that can either be completed by the patient or interviewer and covers Social engagement, Interpersonal communication, Activities of daily living, Recreation, Social activities, Competence at independent living and Occupation/employment.
The literature confirmed that schizophrenia greatly affects quality of life of caregivers. Three publications demonstrated that the QoL of patients with schizophrenia and their caregivers is similar [7,8,31].
According to the literature, QoL significantly improves after a hospital stay, when compared with QoL at the time of admission [30,42]. However, there was no improvement in QoL for additional hospitalization after the initial hospital stay [13,17,28].
2. Stigmatization and discrimination
In addition to a lower QoL, patients with schizophrenia often experienced stigmatization and discrimination, although definitions of the two differed widely among the publications. Negative attitudes towards people with schizophrenia were also found to be prevalent in the CEE countries.
According to both international and country-specific publications, stigma related to schizophrenia can lead to rejection, discrimination, distress, social isolation, unemployment, homelessness, alcohol and drug abuse, and criminalization, factors which reduce the likelihood of clinical improvement and social reintegration [32,44,51]. As a consequence, stigmatization can also lead to poor attitudes towards physical health care, which is associated with higher mortality rates in patients with schizophrenia [52]. Those patients are often treated poorly with regards to their right to work, personal dignity, right to receive legal justice, and equal access to medical treatment [6].
Stigmatization, together with other socioeconomic factors, is a key barrier to employment for patients with schizophrenia [33]. The number of professionally active or studying patients decreases by approximately one-half after initial hospitalization and the majority of patients receive a disability pension, indicating that vocational situation worsens in patients with schizophrenia during the first few years after hospitalization [22].
According to studies that cover populations from more than one country, the level of discrimination against patients with schizophrenia in European countries (including the seven selected CEE countries) was similar. In a multinational study [3], 42% of examined patients reported moderate or high levels of self-stigma (i.e. a personal response to perceived mental illness stigma) and 69% reported moderate-to-high levels of perceived discrimination. The majority of patients felt that the public hold negative attitudes towards mental health service users.
In a Polish study [4], the most common forms of discrimination experienced by patients were listed as: the feeling of being rejected by other people (87%), breaking off personal contact (50%), a negative public image of a mentally ill person in the media (38%), and problems in the area of employment (31%).
The burden of care on families with one or more family member with schizophrenia is very high [33]. Stigmatization and discrimination are key contributors to this burden in both patients with schizophrenia and their caregivers [9,47].
Discussion
A wide variety of QoL publications were identified in this study. In the 37 articles analysed, 15 instruments had been used to assess the impact of schizophrenia on QoL (5 generic and 10 specific to schizophrenia or mental health disorders). Among the general scales, the World Health Organization of Life Instrument BREF (WHOQOL-BREF) (in eight studies) and SF-36 (in six studies) were most frequently used, whilst among schizophrenia-specific scales, QoL was evaluated most often by the Quality of Life Scale (QLS, Heinrichs, in eight studies) and Social Functioning Scale (SFS, Birchwood, in five studies).
A number of aspects of QoL have been investigated and reported in the literature, including:
- factors affecting the QoL of patients with schizophrenia, caregivers or healthy subjects
- factors influencing treatment choice
- correlations with mental condition, psychopathological symptoms or patient functioning.
The studies also differ significantly depending on their purpose, which influences the design, methodology and overall results. Aims of the studies reported are varied but typically include:
- identification of the factors affecting QoL
- comparison of the QoL of patients with schizophrenia versus other patients, caregivers or healthy subjects
- examination of whether QoL is correlated with mental condition, psychopathological symptoms, or patient everyday functioning
- evaluation of the influence of drugs or course of treatment on QoL
Due to the variety of data observed in the studies, it is not possible to make direct comparisons or pool data for analysis. However, it was consistently reported that patients with schizophrenia report worse QoL compared with the general population and that there is a significant negative impact on the QoL of caregivers, such that their QoL is similar to patients with schizophrenia. Furthermore, the QoL of patients with schizophrenia, after inpatient treatment, is significantly better than at time of admission to the hospital.
Conclusion
There has been extensive research into the QoL of patients with schizophrenia and it has been consistently reported that schizophrenia significantly reduces the QoL of patients and their caregivers. In CEE countries, patients with schizophrenia experience stigmatization and discrimination, and an associated impact on their QoL and that of their caregivers. There are a number of tools available to assess QoL, but many of these do not specifically measure the negative symptoms of schizophrenia, which are known to negatively impact QoL. Further research is needed to consolidate the existing body of literature to better understand the drivers of impaired QoL in patients with schizophrenia. In particular, future research could investigate negative symptoms, and how best the burden of illness can be reduced for both patients and caregivers.
Acknowledgements
Editorial assistance for this manuscript was provided by ApotheCom and InVentiv Medical Communications and was funded by F. Hoffmann-La Roche Ltd.
Conflict of Interest
The authors have no conflicts of interest or financial disclosures to declare, however those who are also employees of Roche had support from Roche for their travel to the project meeting, as part of their responsibilities in the project.
Appendix
PRISMA Flow Diagram: Quality of life studies (MEDLINE via PubMed)
- Adamowski T., Hadryś T., Kiejna A.: Comparison between the day-care ward and the in patient ward in terms of treatment effectiveness based onthe analysis of psychopathologic symptoms, subjective quality of life and number of rehospitalisations after discharge. Psychiatr Pol 2008; 42: 571-81
- Awad AG., Voruganti LN.: The burden of schizophrenia on caregivers: a review. Pharmacoeconomics 2008; 26: 149-62
- Brohan E., Elgie R., Sartorius N., Thornicroft G. GAMIAN-Europe Study Group: Self-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: the GAMIAN-Europe study. Schizophr Res 2010; 122(1-3): 232-8
- Cechnicki A., Wojciechowska A.: Zależności pomiędzy właściwościami sieci społecznej a wynikami leczenia osób chorujących na schizofrenię w siedem lat od pierwszej hospitalizacji. [Correlations between features of social network and outcomes in those suffering from schizophrenia seven years from the first hospitalisation]. Psychiatr Pol 2007; 41: 513-25
- Cechnicki A., Wojciechowska A., Valdez M.: Sieć społeczna a jakość życia osób chorujących na schizofrenię w siedem lat od pierwszej hospitalizacji [Social network and quality of life of people suffering from schizophrenia in seven years from first hospitalisation]. Psychiatr Pol 2007; 41: 527-37
- Centrum Badania Opinii Społecznej, Osoby chore psychicznie w społeczeństwie. Komunikat z badań, BS/124/2008 (arr. Wciórka B., Wciórka J.); Available from: www.cbos.pl/SPISKOM.POL/2008/K_124_08.PDF; [Accessed: July 2014]
- Chądzyńska M., Kasperek B., Meder J., Spiridonow K.: Jakość życia osób przewlekle chorych na schizofrenię w ocenie ich samych i ich rodzin [The quality of life of chronic schizophrenic patients in their own and their family's assessment]. Psychiatr Pol 2002; 36: 703-15
- Chądzyńska M., Spiridonow K., Kasperek B., Meder J.: Porównanie jakości życia osób chorych na schizofrenię i ich opiekunów [Quality of life of schizophrenic patients and their caregivers--comparison]. Psychiatr Pol 2003; 37: 1025-36
- Chrząstowski S: Związki między brzemieniem rodziców osób z rozpoznaniem schizofrenii lub zaburzeń osobowości a kształtowaniem się relacji w rodzinie [Links between burden of care in parents of patients with schizophrenia or personality disorders and family interactions]. Psychiatr Pol 2006; 40: 901-11
- Czernikiewicz A, Górecka J: Porównanie subiektywnej i obiektywnej oceny jakości życia w grupie chorych na schizofrenię [Comparison of subjective and objective quality of life in a group of schizophrenic patients] Psychiatr Pol 2003; 37: 669-81
- Czernikiewicz A, Górecka J, Kozak-Sykała A: Przystosowanie przedchorobowe, a jakość życia chorych na schizofrenię [Premorbid adjustment and quality of life in schizophrenia] Pol Merkur Lekarski 2005; 19: 659-62
- De Marinis TD, Saleem PT, Glue P, Arnoldussen WJ, Teijeiro R, Lex A et al.: Switching to long-acting injectable risperidone is beneficial with regard to clinical outcomes, regardless of previous conventional medication in patients with schizophrenia. Pharmacopsychiatry 2007; 40: 257-63.
- Dernovsek MZ, PrevolnikRupel V, Rebolj M, Tavcar R: Quality of life and treatment costs in schizophrenic outpatients, treated with depot neuroleptics. Eur Psychiatry 2001; 16: 474-82.
- Główczak M, Kasperek B, Meder J, Spiridonow K: Wstępna ocena jakości życia pacjentów przewlekle chorych z rozpoznaniem schizofrenii [The preliminary evaluation of quality of life in patients with chronic schizophrenia] Psychiatr Pol 1997; 31: 313-22.
- Golubovic B, Misic-Pavkov G, Gajic Z, Ivanovic-Kovacevic S: Evaluation of quality of life for patients with schizophrenic and schizoaffective disorders related to the use of antipsychotic therapy. Med Arh 2010; 64: 37-40
- Górecka JE, Czernikiewicz A: Związek jakości życia chorych na schizofrenię z parametrami klinicznymi psychozy [The relationship between quality of life of schizophrenic patients and clinical parameters of psychosis] Wiad Lek 2004; 57: 408-12
- Górna K, Jaracz K, Rybakowski F: Objective and subjective quality of life in schizophrenic patients after a first hospitalization. Rocz Akad Med Bialymst 2005; 50 Suppl 1: 225-7
- Górna K, Jaracz K, Rybakowski F, Rybakowski J: Determinants of objective and subjective quality of life in first-time-admission schizophrenic patients in Poland: a longitudinal study. Qual Life Res 2008; 17: 237-47
- Górna K, Jaracz K, Wrzyszczyńska L, Rybakowski F: Quality of life and depression in schizophrenic patients. Adv Med Sci 2007; 52 Suppl 1: 108-11
- Hanuszkiewicz I, Cechnicki A, Kalisz A: Badania wstępne uczestników programu rehabilitacyjnego [Correlation between cognitive defects and the course of schizophrenia. Initial study of a rehabilitation programme participants]. Psychiatr Pol 2007; 41: 539-50
- Jackowska E: Stygmatyzacja i wykluczenie społeczne osób chorujących na schizofrenię - przegląd badań i mechanizmy psychologiczne [Stigma and discrimination towards people with schizophrenia--a survey of studies and psychological mechanisms]. Psychiatr Pol 2009; 43(6): 655-70
- Jaracz K, Górna K, Kiejda J, Rybakowski J: Prospektywna ocena wczesnego przebiegu schizofrenii u kobiet i mężczyzn po pierwszej hospitalizacji psychiatrycznej [Prospective evaluation of the early course of schizophrenia in men and women after a first psychiatric hospitalization]. Psychiatr Pol 2008; 42: 33-46
- Jarema M, Konieczyńska Z: Badanie jakości życia a efekty farmakoterapii schizofrenii lekami klasycznymi i “starymi” atypowymi [Quality of life in schizophrenic patients treated with classic and "old" atypical neuroleptics]. Psychiatr Pol 2000; 34: 275-88
- Jarema M, Bury L, Konieczyńska Z, Zaborowski B, Cikowska G, Kunicka A et al.: Porównanie oceny jakości życia chorych na schizofrenię objętych różnymi formami opieki psychiatrycznej [Comparison of quality of life of schizophrenic patients in different forms of psychiatric care]. Psychiatr Pol 1997; 31: 585-94
- Jarema M, Konieczyńska Z, Główczak M, Szaniawska A, Meder J, Jakubiak A: Próba analizy subiektywnej oceny jakości życia pacjentów z rozpoznaniem schizofrenii lub depresji [The evaluation of subjective quality of life in patients with schizophrenia or depression]. Psychiatr Pol 1995; 29: 641-54
- Jarema M, Konieczyńska Z, Murawiec S, Szafranski T, Szaniawska A: Zmiana jakości życia i obrazu klinicznego w schizofrenii [The change of quality of life and clinical picture in schizophrenia]. Psychiatr Pol 2002; 36: 393-402
- Jukić V, Barić V, Čulav-Sumić J, Herceg M, Majdančić Ž, Werft-Čop M: The impact of novel antipsychotic drugs on quality of life among people suffering from schizophrenia. Coll Antropol 2003; 27 Suppl 1: 119-24
- Kasperek B, Spiridonow K, Chądzyńska M, Meder J: Jakość życia chorych na schizofrenię a umiejętność rozwiązywania problemów związanych z chorobą - porównanie grup pacjentów uczestniczących w treningu behawioralnym i psychoedukacji [Quality of life of schizophrenia patients and health related problem solving skills--comparison between the group of patient participated in social skills training and psychoeducation group]. Psychiatr Pol 2002; 36: 717-30
- Konarzewska B, Waszkiewicz N, Szulc A, Łazarczyk-Kirejczyk J, Małus A: Nadużywanie alkoholu w rodzinie - objawy depresyjne oraz subiektywna ocena jakości życia a wyniki w skali MAST u pacjentów z rozpoznaną schizofrenią i alkoholizmem [Family history of alcohol abuse - depressive symptoms and the quality of life in view of the MAST score of schizophrenic patients with dual diagnosis]. Pol Merkur Lekarski 2012;33:147-50
- Konieczyńska Z, Jarema M, Cikowska G: Badanie jakości życia zależnej od stanu zdrowia chorych leczonych z powodu schizofrenii na oddziale dziennym [Evaluation of health-related quality of life in schizophrenic patients from day hospital]. Psychiatr Pol 1997; 31: 323-32
- Margetić BA, Jakovljević M, Ivanec D, Margetić B: Temperament, character, and quality of life in patients with schizophrenia and their first-degree relatives. Compr Psychiatry 2011; 52: 425-30
- Margetić BA, Jakovljević M, Ivanec D, Margetić B, Tošić G: Relations of internalized stigma with temperament and character in patients with schizophrenia. Compr Psychiatry 2010; 51: 603-06
- Marwaha S & Johnson S: Schizophrenia and employment - a review. Soc Psychiatry Psychiatr Epidemiol 2004; 39(5): 337-49
- McGorry P: Royal Australian and New Zealand College of Psychiatrists Clinical Practice Guidelines Team for the Treatment of Schizophrenia and Related Disorders. Aust N Z J Psychiatry 2005; 39: 1-30
- Mihajlović G, Jovanović-Mihajlović N, Radmanović B, Radonjić K, Đukić-Dejanović S, Janković S et al.: Quality of life of schizophrenic patients treated with haloperidol depot and injection preparation of long-lasting risperidone. Srp Arh Celok Lek 2011; 139 Suppl 1:36-40
- National Collaborating Centre for Mental Health UK. (2014): Psychosis and Schizophrenia in Adults: Treatment and Management. National Institute for Health and Care Excellence (NICE) Clinical Guideline 178. February 2014; Available from: http://www.nice.org.uk/guidance/cg178/resources/guidance-psychosis-and-schizophrenia-in-adults-treatment-and-management-pdf ; [Accessed December 2014]
- Opalić P., Femić N.: Istraživanje kvaliteta života obolelih od shizofrenije u Beogradu [Research of the quality of life of schizophrenic patients in Belgrade] Med Pregl 2008; 61: 625-31
- Pąchalska M, Kiejna A, Frańczuk B, Talar J, Silverman F H, Grochmal-Bach B, & Macqueen BD: Post-coma paraschizophrenia and quality of life in patients with closed-head injuries. Ortop Traumatol Rehabil 2001; 3: 401-11
- Péntek M, Harangozó J, Egerházi A, Kelemen O, Gulácsi L, Baji P et al.: [Health related quality of life and disease burden of patients with schizophrenia in Hungary]. Psychiatr Hung 2012; 27: 4-17
- Pesek MB, Mihoci J, Medved K & Šolinc NP: Long term groups of patients with psychosis: physical activity and medical treatment Psychiatr Danub 2011; 23 Suppl 1: 149-54
- Pesek MB, Mihoci J, Šolinc NP, Avguštin B: Long term groups for patients with psychosis in partial remission - evaluation of ten years' work. Psychiatr Danub 2010; 22 Suppl 1: 88-91
- Popławska R, Czernikiewicz A, Szulc A, Galińska B, Konarzewska B, Rudnik-Szałaj I: Ocena efektywności psychoedukacji w grupach pacjentów psychotycznych I depresyjnych - badanie pilotażowe [The effectiveness of psychoeducation in schizophrenic and depressive patients -preliminary report]. Psychiatr Pol 2004; 38: 433-42
- Priebe S, McCabe R, Schützwohl M, Kiejna A, Nawka P, Raboch J et al.: Patient characteristics predicting better treatment outcomes in day hospitals compared with inpatient wards. Psychiatr Serv 2011; 62: 278-84
- Rössler W, Salize HJ, van Os J, Riecher-Rössler A: Size of burden of schizophrenia and psychotic disorders. Eur Neuropsychopharmacol 2005; 15: 399-409
- Ružić K., Frančišković T., Šuković Z, Žarković-Palijan T, Buzina N, Rončević-Gržeta I: Predictors of aggressiveness in schizophrenic patients treated in inpatient forensic institutions. Coll Antropol 2008; 32: 331-37
- Spiridonow K., Kasperek B., Meder J.: Porównanie subiektywnej jakości życia pacjentów przewlekle chorych z rozpoznaniem schizofrenii i osób zdrowych [Subjective quality of life in patients with chronic schizophrenia and in healthy persons] Psychiatr Pol 1998; 32: 297-306
- Świtaj P., Wciórka J., Grygiel P., Smolarska-Świtaj J., Anczewska M., Grzesik A: Experience of stigma by people with schizophrenia compared with people with depression or malignancies. Psychiatrist 2011; 35: 135-9
- Świtaj P., Anczewska M., Chrostek A., Sabariego C., Cieza A., Bickenbach J et al.: Disability and schizophrenia: a systematic review of experienced psychosocial difficulties. BMC Psychiatry 2012; 12: 193
- Tomczak P.: Poszerzone badania nad religijnością pacjentów z rozpoznaniem schizofrenii [Religiousness of patients with diagnosis of schizophrenia. Wide-ranging studies]. Psychiatr Pol 2006; 40: 885-99
- Tomczak P.: Religijność pacjentów z rozpoznaniem schizofrenii. Wstępne ustalenia korelacyjne i porównawcze z osobami bez zaburzeń [Religiousness of patients with diagnosis of schizophrenia. Introductory studies]. Psychiatr Pol 2005; 39: 869-81
- Vidojević IM, Jočić DD., Tošković O:. Comparative study of experienced and anticipated stigma in Serbia and the word. Int J Soc Psychiatry 2011; 58: 355-61
- Wildgust HJ., Beary M,: Are there modifiable risk factors which will reduce the excess mortality in schizophrenia? J Psychopharmacol 2010; 24(4 Suppl): 37-50