Telemedicine - a miracle cure for everything?
-
Copyright
© 2016 PRO MEDICINA Foundation, Published by PRO MEDICINA Foundation
User License
The journal provides published content under the terms of the Creative Commons 4.0 Attribution-International Non-Commercial Use (CC BY-NC 4.0) license.
Authors
Background: Telemedicine is an interesting area of modern treatment. It enables contact between patients and doctors at long distance. In this paper, we present the latest studies, conducted among Polish doctors about the utility of the telemedicine as a therapeutic tool.
Methods: One of the methods was an anonymous questionnaire presented to psychiatrists from Poland (105 physicians). The second study was based on a questionnaire filled by participants (scale: 1-inappropriate to 5-very useful). It was part of the Polish Telemedical Project (grant no.POIG.01.04.00-04-219/12) conducted to assess medical Platform ‘Moneo’ in the therapy of the areas other than psychiatry.
Results: All healthcare institutions noticed advantages of Medical Platform. The Platform’s functionalities, rated as the best by healthcare directors were: educational materials, appointment and therapy planning. Managers indicated parts which could be improved in e-prescribing system, the process of collecting information about hospitalizations, operations. Functionalities regarded by doctors as desirable in improving the platform include: e-prescribing system, reporting side effects, planning visits, educational materials.
In the psychiatrists' study, they had confirmed the potential of telemedicine in psychiatry. They chose mood and neurotic disorders as the most adequate for that treatment. However, 60% of doctors would not widen the implementation of telepsychiatry in Poland. Probably it is due to their awareness for the need of new software, legal and refunding system.Conclusion:
Telemedicine is a useful method for specialists and directors. It can improve quality of healthcare services. However, lots of improvements in telemedical services are needed to make it a miraculous cure for everything.Introduction
Telemedicine is a very interesting area of modern treatment, using a comprehensive spectrum of communication technologies. As the prefix ‘tele’ suggests, it enables the contact between patients and doctors no matter what the distance is, via e-mail, SMS or videoconferencing. Additionally, it consists of web pages with data about diseases and their therapy, video- and audiobooks, which patients can use at home. Contemporarily, videoconferencing has become the mainstream in telemedicine treatment and other forms defined as e-health. The main objective of telemedicine is to save time, improve access to professional treatment for all patients, remind patients of health goals, make appointment planning as well as therapy homework more efficient [1].
Modern telemedicine has begun with experiments, conducted to provide medical services evenly to everybody, such as those by Willem Einthoven’s 1905 long distance transfer of electrocardiograms, through the era of teleradiology and telepsychiatry of the 1950s. The development of telemedicine matured in the 1990s and has reached its final in the adoption to the present technology [2].
Nowadays, telemedicine is a proven way to improve patients’ attendance at appointments and it has positive effects on patients with chronic diseases [3,4]. Efforts to make telemedicine part of common treatment in Poland are still in process. Reliable web pages are being developed day by day, however, there are still some problems with communication, concerning fear of abuse, lack of knowledge in practitioners, lack of actual law regulations and financial support from the health system [5]. Due to the lack of researches on acceptance and attitude of Polish professionals towards telemedicine, we decided to conduct two studies on utility of the telemedicine as a therapeutic tool in different medical specialties.
Materials and Methods
The aim of the study was to examine doctors’ attitude to telemedicine. The first study was part of the Polish telemedical project, granted from National Center for Research and Development (grant no.POIG.01.04.00-04-219/12) conducted to assess medical Platform Moneo as a therapeutic tool in the therapy of the areas other than psychiatry. It also serves to evaluate the potential ability of introducing this to standard therapy. Method of the study was based on a questionnaire filled with the use of a scale scored from 1 to 5, where 1 means “unsuitable” and 5 “very useful”. The survey was directed at the staff of health care management: individual medical practice (25 people), private health care center (25 people), state hospitals (25 people), private hospitals (25 people) - Giving us a total of one hundred people from Poland. The survey was also dedicated to 12 specialist doctors.
The second study was based on authors’ anonymous questionnaires distributed amongst psychiatrists from Poland (105 doctors aged 26-74, including 74 women and 31 men).
Table 1.
| Polish Telemedical Project | Study about telepsychiatry in Poland | |
| Study group | 1) Cardiologists2) Urologists3) Pulmonologists4) Managers | 1) Psychiatrists2) Psychiatric Patients **** |
| The number of respondents | 4) 100*, 12** | 1) 1052) 102 |
| Method | Evaluative research with the use of CATI *** | Anonymous survey |
* The survey was directed at the personnel of health care management: Individual medical practice (25 people), Private health care center (25 people), State hospitals (25 people), Private hospitals (25 people) - Giving a total one hundred people from whole Poland.
** The survey was also dedicated to 12 specialist doctors.
*** Computer Assisted Telephone Interview; realized with the use of information tools based on CATI study script from 13.10.2014, without patients’ participation.
**** Patients of the Department of Psychiatry and Psychotherapy of Medical University of Silesia.
Results
Managers
All healthcare institutions noticed advantages of the possibility of using Medical Platform as a therapeutic tool. In the question which estimates currently available Platform functionalities, in an individual medical practice group ‘educational materials’ received the highest grade (average 4.12). For private health care centers ‘planning appointments’ was the best option (average 4.36) and in public and private hospitals it was ‘therapy planning’ - it received the best score (average 4.24). The worst rated was the concept of ‘videoconference’ (average 3.04) and ‘examination using clinical scales’, it was rated at the lowest level (2.92).
Table 2.
| Individual medical practice | Private health care center | State hospital | Private hospital | |
| >4 | educational materials | appointments’ planning | therapy planning, educational materials, appointments’ planning, side effects reporting | therapy planning, educational materials, appointments’ planning, side effects reporting |
| 3 -4 | therapy planning , compliancemeasurement, appointment planning, side effects reporting | video conference | video conference | examination with the use of clinical scales |
| <3 | report about clinical factors, examination with the use clinical scales |
As regards the question about proposals for improving the Platform, considered as “useful” or “very useful” (average more than 4) the following were approved: ‘improvement of e-prescribing system’ (4.12), ‘collection of information about hospitalizations of the patient’ (4.07), ‘collection of information about operations’ (4.05). Only options ‘entering the results of laboratory tests by the patient/guardian’, ‘monitoring patient’s physical activity’ and ‘monitoring the patient's diet’ received on average less than 3 points.
Opinions of the management of health care institutions, concerning the possibility of employment of telemedicine were divided (average score 2.71). The level of interest in the offered solutions fluctuated around 2.45. The situation was similar when assessing charging fees for using the telemedicine. Majority of respondents, i.e. 61%, rated this possibility in the range of 1-2 (average 2.25).
Managers were unanimous in evaluating the amount of first-time visits that could be done through the Platform - 84% of respondents indicated range of 0-20%. In the case of follow-up visits, opinion of respondents were divided, but majority of respondents (89%) do not see the possibility that more than 60% of the visits could be done through the Platform.
As regards the question: "Have you noticed the need of the introduction of telemedicine services in patients aged more than 65 years?", responses were split in proportion to each level of the 5-point scale. The average was 2.93. However, the possibility of implementing the Platform in patients aged more than 65 years was rated more critically (average 2.36).
In the presented analysis, this Platform received the highest rate from the management of private hospitals, while the lowest mark was given by the management of private practices. Evaluation obtained from Non-public Health Care Centre and public hospitals were very similar.
Pulmonologists, cardiologists and urologists
The survey was used as a tool for evaluating the available opportunities to use the Platform: videoconferences, clinical examination scales, cognitive training, treatment planning, compliance measurement, educational materials, visit planning, reports about clinical parameters and side effects reporting (1-5 rating scale). It also allowed us to gather suggestions regarding optimization.
The average rate of all tested possibilities of the Platform was evaluated as more than useful (average score 4.13) in conducting treatment by pulmonologists (4.3), cardiologists (4.11) and urologists (3.97). The most frequently chosen functionality was ‘planning visits’ (4.67), ‘videoconference’ then ‘treatment planning’ (4.58), then ‘compliance measurement’ (4.33) and then ‘educational materials’ (4.08). The most uncommonly selected component was ‘clinical reports’ (3.58).It is worth emphasizing that the average assessment of individual medical specializations did not differ among themselves.
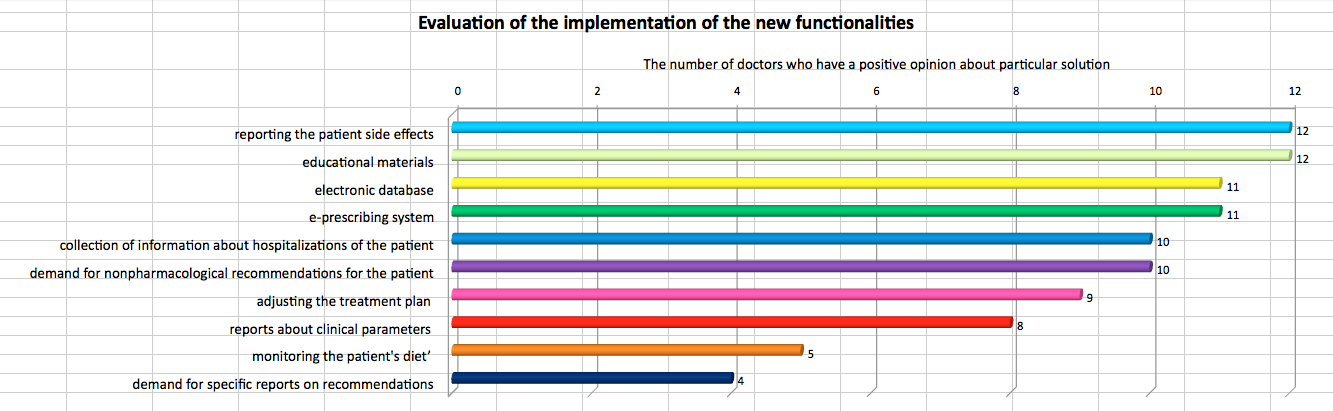
Functionalities regarded by doctors as desirable to increase the utility of the Platform are: ‘e-prescribing system’, ‘reporting the patient side effects’, ‘visits planning’, ‘educational materials’ dedicated to different groups of patients.
The next step was to gather suggestions regarding the preferences and expectations of doctors about the possible use of telemedicine and information that could be provided through the Platform.
According to cardiologists, the Platform could be supplemented with i.a. reporting of clinical parameters, compliance measurement, videocommunication plus clinical scale examination, nonpharmacological recommendations for patients, the results of laboratory and diagnostic tests and monitoring of the therapy. Cognitive training, the need for specific reports regarding nonpharmacological recommendations, monitoring diet and activity of the patient were evaluated as unnecessary for further development
According to urologists, the Platform should be expanded in the following fields: assessment of symptoms (using e.g. the IPSS scale, which is used to rate the severity of symptoms among patients with urination disorders in the course of benign prostatic hyperplasia). Furthermore, it is recommended that clinical scales appropriate for a specific group of patients be introduced. It is also desirable to develop educational materials dedicated to different groups of patients.
Optimization of the platform at the pulmonological level should include: opportunity of conversation between doctor and patient, self-measurement of PEF, opportunity to make an appointment, transfer of treatment scheme and its changes during observation of the patient, compliance’s check, disease control (ACT test - patients with asthma, COPD assessment test - in the context of chronic obstructive pulmonary disease) and patients’ education (lectures about diseases, their treatment and prevention (quitting smoking, avoiding allergens etc.)) and wide range of presentations (for example drug inhalation technique).
Psychiatrists
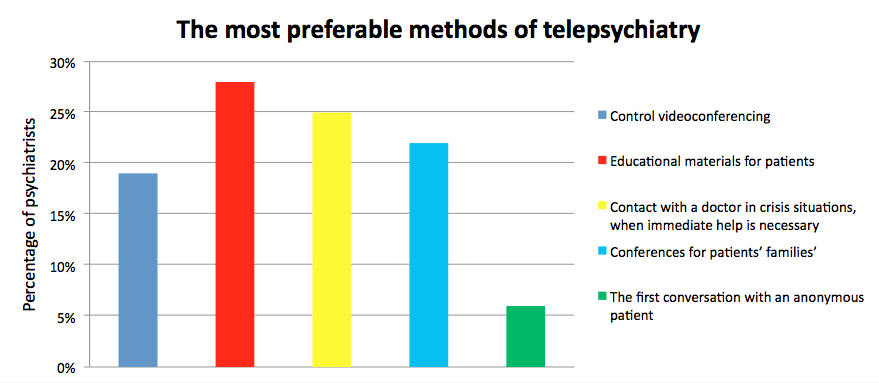
According to the study conducted amongst psychiatrists, only 15% of them claim to have an extensive knowledge on telepsychiatry, 76% has a general knowledge about it, 6% heard about it but do not know what it means, and 3% never heard of it. Merely 16% of doctors used telepsychiatry, 84% never tried it [5]. Vast majority of the respondents perceive telepsychiatry as a useful method of treatment in many situations. Almost all of them evaluate this method as a potential complement to conventional therapy. As seen on the diagram, the most preferable methods of telepsychiatry chosen by psychiatrists were ‘educational materials for patients’. In second place came ‘contact with a doctor in crisis situations, when immediate help is necessary’, and the last on podium was ‘conferences for patients’ families’. ‘Control videoconferencing’ was fourth, and ‘the first conversation with an anonymous patient’ came in as least popular.
According to the physicians, telepsychiatry would be most effective in mood and neurotic disorders (wherein men did not take it into account) and less effective in mental disabilities and mental development disorders. Majority of older doctors, despite their greater willingness to introduce telepsychiatry, could not bring up any disease in which telepsychiatry might be useful. Although doctors noticed positive aspects of this method, 60% of them would ignore its widespread implementation in Poland. Simultaneously, 60% of physicians claim that if they had an opportunity to try telepsychiatry, they would do that. Furthermore, most doctors claim that this method would be particularly useful for people living far away from hospital.
However, these doctors strongly agreed that before common insertion of this method, legal- and refunding system changes should be made. They also noted the need of new software. Simultaneously they were concerned about the disclosure of personal data, the loss of medical secrecy and abuse of this method by patients.
Discussion
Telemedicine as the cure
The World Health Organization defines telemedicine as beneficial use of information and communication technology in the support of health and healthcare [6]. Accordingly, despite all differences between these two aforementioned studies, both of them suggest that telemedicine is a valuable method worth implementing in Polish medical service. Psychiatrists, together with urologists, pulmonologists, cardiologists and managers unanimously perceive telemedicine as useful in treatment. Administrators and psychiatrists consider ‘educational materials’ as the most useful functionality. On the other hand, the first group agrees with the specialists that ‘planning appointments’ is an extremely convenient one too. Psychiatrists also confirmed that telemedicine would be useful in therapy of a wide range of psychiatric ailments, especially mood and neurotic disorders. As proven in many publications, telemedicine is an effective medical tool used to cure a comprehensive spectrum of diseases in almost every medical specialty. In psychiatry: e.g. schizophrenia was treated with great success [7], dermatology [8], radiology, cardiology and even stomatology [9]. Telemedicine is used in treatment of both chronic diseases [10,11] and sudden cases [12,13]. It is also confirmed that this method can be used in adults [14] as well as children and neonates [15].
All arguments mentioned earlier confirm that this technique is not only a cure for patients but also a profitable medium to improve healthcare service and patients’ self-awareness, as well as to make prevention more effective.
Telemedicine as the miracle
For some people telemedicine is the only chance to consult a doctor, and as proven by a group of scientists from India [16] it is an effective method of treatment for people living in high mountains. From this perspective, telemedicine could be considered a miracle of application of contemporary technologies to bring help to patients inaccessible by traditional medicine.
Telemedicine is not the cheapest and easiest method to implement in the world, although this treatment method can be cheaper than traditional methods without losing its effectiveness. That fact was proven in the study on two groups of general practitioners, who had similar patients, and the direct cost of the visit to an outpatient clinic in internal medicine turned out seven times greater per patient than those of an electronic consultation [17]. Additionally, this insertion requires legal and refunding system changes, which might become more difficult than introduction of the method itself. Those problems had been noticed by psychiatrists. Doctors and managers have given the opportunity to propose improvements such as compounding the system with the possibility to use clinical scales to asses patients and of reporting patients’ side effects. Thus, telemedicine has a potential to be a real miracle, but as all miracles it needs convenient conditions to actually become one.
Conclusions
Considering all data, telemedicine is a useful method for specialists and for directors. It can improve healthcare service and make an access to it possible for some people. However, it might be implepented in Poland too only if some effort will be made to introduce legal and refunding system changes as well as improvements in telemedical services, especially in terms of expanding it by adding more fields of action.
- Klasnja P,Pratt W. Healthcare in the pocket: mapping the space of mobile-phone health interventions. Journal of Biomedical Informatics. 2012; 45:184–98
- Bashshur RL, Shannon GW, Smith BR., et al. The empirical foundations of telemedicine interventions for chronic disease management. Telemedicine and e-Health. 2014; 20(9):769
- Hasvold PE, Wootton R. Use of telephone and SMS reminders to improve attendance at hospital appointments: a systematic review. Journal of Telemedicine and Telecare. 2011; 17:358–364
- Wootton R. Twenty years of telemedicine in chronic disease management – an evidence synthesis. Journal of Telemedicine and Telecare. 2012; 18:211–220
- Wojtuszek M, Kachnic J, Krysta K, Wutke J. Telepsychiatry in Polish patients’ and doctors’ opinion. Psychiatria Danubina, 2015; 27(1): 379–382
- WHO. Telemedicine opportunities and developments in member states - Report on the second global survey on eHealth Global Observatory for eHealth series. 2010; 2:96.=
- Kasckow J, Felmet K, Appelt C, Thompson R, Rotondi A, Haas G. Clinical Schizophrenia and Related Psychoses. 2014; 8(1):21-27
- Wurm EM, Hofmann-Wellenhof R, Wurm R, Soyer HP. Telemedicine and teledermatology: past, present and future; Journal of the German Society of Dermatology: JDDG 2008; 6(2):106-12
- Boringi M, Waghray S, Lavanya R, et al. Knowledge and awareness of teledentistry among dental professionals - a cross sectional study; Journal of Clinical and Diagnostic Research 2015; 9(8):C41-4
- Whitten P, Collins B, Mair F. Nurse and patient reactions to a developmental home telecare system. Journal of Telemedicine and Telecare. 1998; 4:152–160
- Wootton R. Recent advances: Telemedicine. British Medical Journal. 2001; 323(7312):557-560
- Skorning M, Bergrath S, Rörtgen D, et al. E-health in emergency medicine - the research project Med-on-@ix. Anesthetist. 2009; 58(3):285-92
- Brennan JA, Kealy JA, Gerardi LH, et al. A randomized controlled trial of telemedicine in an emergency department. Journal of Telemedicine and Telecare. 1998; Supp 1; 4: 18
- Shores MM, Ryan-Dykes P, Williams RM, et al. Identifying undiagnosed dementia in residential care veterans: comparing telemedicine to in-person clinical examination. International Journal of Geriatric Psychiatry. 2004; 19(2): 101–108
- Robinson C, Gund A, Sjöqvist BA, Bry K. Using telemedicine in the care of newborn infants after discharge from a Swedish neonatal intensive care unit reduced the need of hospital visits.Acta Paediatrica 2016; 21. doi: 10.1111/apa.13407
- Ganapathy K, Chawdhry V, Premanand S, et al. Telemedicine in the Himalayas: operational challenges - a preliminary report. Telemedicine and e-Health. Telemedicine Jurnal e-Health. 2016
- Harno K, Paavola T, Carlson C, Viikinkoski P. Patient referral by telemedicine: effectiveness and cost analysis of an intranet system. Journal of Telemedicine and Telecare. 2000; 6:320–329