Diabetic Macular Edema treatment limits in Poland
-
Copyright
© 2016 PRO MEDICINA Foundation, Published by PRO MEDICINA Foundation
User License
The journal provides published content under the terms of the Creative Commons 4.0 Attribution-International Non-Commercial Use (CC BY-NC 4.0) license.
Authors
Diabetic Macular Edema (DME) is a severe disease, related to Diabetic Retinopathy (DR). All diabetic patients are at risk of DME development. The disease severity may vary from mild to moderate, with a risk of loss of vision. Diabetic Retinopathy, including Diabetic Macular Edema patients in Poland, are treated within Diagnosis Related Groups (JGP) system, that allows settlement of costs of performed medical procedures, including vitreoretinal procedures, fotocoagulation, and administration of VEGF inhibitors.
In this article authors tried to analyse what are the costs of treatment of DME patients within Diagnosis Related Groups (JGP) in Poland, what are the trends in expenditures of DME treatment, and what are the recommended steps to the decision makers in vision loss prevention amongst mellitus patients in Poland?
The study and analyses in this article are based on Diagnosis Related Groups (JGP) statistical reports available for years 2009-2015, published by the Polish National Health Fund (NFZ).
DME treatment spendings within the JGP groups in Poland, are notably low, vary from 1,2 MM PLN in 2009, achieving its maximum of 1,5MM PLN in 2010, and resulting in <1,1 MM PLN in year 2015. The number of treated patients decreased markedly from more than 800 in year 2009, achieving its minimum of 198 patients in year 2014.
DME treatment in Poland within the public system is remarkably below needs, and it does not meet standards of vision loss prevention amongst mellitus patients. The situation is mainly caused by under-diagnosis at the primary healthcare outpatient clinics, long waiting time for an ophthalmologist consultations and treatment budget limits within JGP groups in hospitals.
Diabetic Macular Edema (DME) is a severe disease, related to the Diabetic Retinopathy (DR). All diabetic patients are at risk of DME development. The disease severity may vary from mild to moderate, with risk of loss of vision. 25% to 30% non ophthalmology treated, and up to 15% ophthalmology treated diabetic patients might be affected by moderate loss of vision due to DME. Based on the Rohit Varma, Neil M. Dressler study published in JAMA Ophthalmology weighted DME prevalence in USA is 3,8% (2.7%-4.9%) of diabetes, however the meta-analysis of 35 studies (22,896 patients from United States, Australia, Europe and Asia) calculates DME prevalence on 7.48% (7.39–7.57) of the overall diabetes population.
Progression to DME affects 3% of mild non-proliferative DR eyes, 38% moderate and severe non-proliferative DR eyes and relates up to 71% eyes of the proliferative Diabetic Retinopathy - the most vision-threatening form of the disease,.
According to the Los Angeles Latino Eye Study and in the Proyecto VER study - 18% of participants with diabetes of more than 15 years’ duration had the proliferative DR, with no PDR percentage difference between Type 1 vs Type 2 diabetes.
Polish National Health Fund (NFZ) estimates diabetes patients on 2 millions in Poland. Based on NFZ data and referring to cited above Rohit Warma as well as Joanne Yau studies, authors calculate DME prevalence from 76.000 to 149.000 patients in Poland.
In this article authors tried to assess what are the Diabetic Macular Edema treatment limits in a Polish healthcare system perspective.
To answer this question, the Polish National Health Fund (NFZ), Diagnosis Related Group (JGP) data were used. For any other calculations in this article, authors accounted 7,48% DME prevalence amongst mellitus patients as the most relevant to Poland.
NFZ regularly publishes JGP statistics, and since year 2009, there are specific common treatment baskets relevant to eye diseases (JGP B1 to B98).
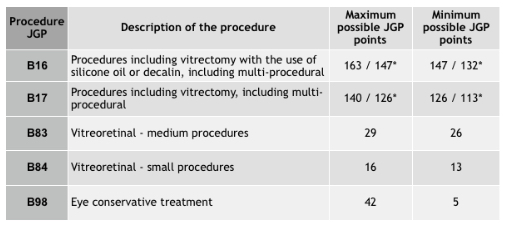
As for the ICD-10 classification, Diabetic Retinopathy H 36.0 with ICD-9 procedures (E10-E14) are included in NFZ hospital JGP statistics presented in the table 1.
*from year 2016
Based on the above information, we can observe that during Diabetic Retinopathy treatment in hospitals in Poland, ophthalmologists utilise B16, B17, B83, B84 and B98 JGP groups in order to settle the costs of a treatment, however the value of groups significantly differ in points. Taking into account that 1 hospital JGP point equals to approximately 52 Polish Zloty, DR treatment in years 2009 - 2015 were being settled on value from minimum 260 PLN, up to 8.476 PLN depending on list of medical ICD-9 procedures within a JGP group and type of a hospitalisation performed (‘full’ hospitalisation, planned hospitalisation, 1 day hospitalisation).
All the presented JGP statistics in the NFZ JGP platform do not cover specifically Diabetic Macular Edema, fortunately there are available Diabetic Retinopathy hospitalisation data, so for the purposes of this article, authors have included all cited above outcomes of the DR and DME medical studies.
To calculate Diabetic Macular Edema treatment costs, based on the available JGP data, we propose to use a mathematical formula, directly related to DME progression to non-proliferative and proliferative Diabetic Retinopathy (H 36.0). The formula is presented as below:
DME Hospitalisations = DR Hospitalisations *((82%*38%) + (18%*71%))
Where:
82% - non-proliferative patients ratio amongst Diabetic Retinopathy
18% - proliferative patients ratio amongst Diabetic Retinopathy
38% - non-proliferative moderate and severe DR eyes ratio
71% - proliferative DR eyes ratio
Using the formula it can be estimated a number of DME hospitalisations and DME patients.
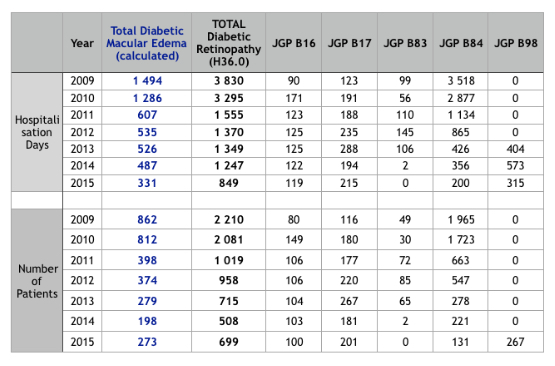
Diabetic Retinopathy, calculated Diabetic Macura Edema JGP hospitalisations and number of treated patients are presented in the table 2.
Analysing the number of the DR and DME hospitalisations, as presented in the table 2, we can remark that, the number of DR and DME treated patients within the JGP groups is significantly low. As described above, in Poland there are approximately 2 millions of diabetes patients, and referring to Joanne W.Y. Yau, DME prevalence as of 7.48% of the overall diabetes population, the number of DME patients equals to around 149.000. Considering that about 50% of them have moderate and severe symptoms of DME, it looks like that in order to achieve high level of vision loss prevention amongst DME patients, ophthalmologist in Poland would have to intensively treat at least 2000 patients per year. Currently there is a huge gap, between a number of treated patients within the public healthcare system versus treatment needs that would prevent worsening or even loss of vision amongst mellitus patients.
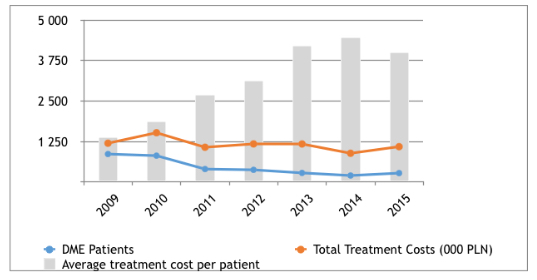
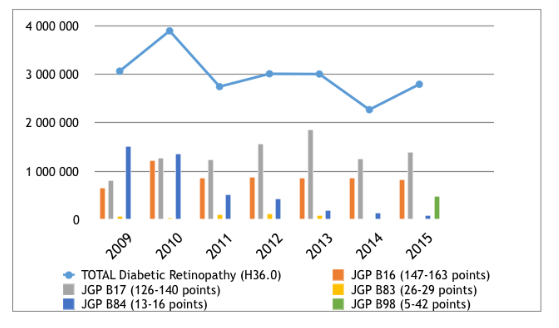
Like in other diseases in Poland, there may be some budget limitations, that reduces level of treatment due to potential high cost of treatment to the healthcare system. To answer this doubt, there are calculated DR and DME patients costs of treatment within the JGP groups, presented in the figure 1.
According to the data presented in the figure 1, authors observe a stable, low annual treatment costs for DME patients treated within the JGP groups. The spendings vary from 1,2 million PLN in 2009, achieving its maximum of 1,5 million PLN in 2010, and resulting in less than 1,1 million PLN in year 2015. Simultaneously the number of treated patients decreased markedly from more than 800 in years 2009 and 2010, to close to 400 in years 2011 and 2012, achieving its minimum of 198 patients in year 2014. Constant costs of treatment with decreasing trend of treated patients resulted boosting average cost treatment per 1 statistical DME patient.
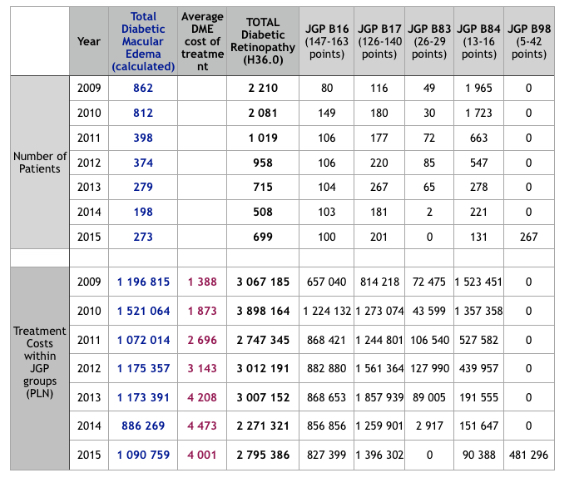
The calculation of the number of treated patients, average cost of treatment and total costs of treatment of DME patients within the JGP system are presented in the table 3.
As per table 3 presented data, authors conclude, that the root cause of significant decrease of DR and DME treated patients with simultaneously kept overall expenditures is mainly caused by giving up treatment within less valued JGP groups as of B83 and B84. Especially in the JGP group B84 there is a drop of treated patients from almost 2000 in year to 2009 to barely 131 patients in year 2015. Within this procedure a laser fotocoagulation is available for the treatment only. On the other hand, within the JGP procedure B98, where there is a possibility to administer VEGF inhibitor, in year 2015 ophthalmologists started to treat 267 DR patients. The most valued JGP groups B16 and B17 have kept the level of treated patients over the discussed period of years 2009 - 2015.
Trend of DR treatment costs within JGP groups is presented in the figure 2.
Discussion
This study aimed to show, what are the DME treatment costs in Poland, based on NFZ JGP statistics. The results show, small and decreasing number of treated DME patients within the JGP groups in Poland which is contrary to the disease prevalence and treatment needs that should focus on vision loss prevention amongst diabetes mellitus patients. However, the current JGP system points within the groups as of B16, B17, B83, B84 and B98 allows DME treatment, but in fact the valuation of a group, consisting form ICD-9 procedures is not directly linked with DME treatment (in opposite to i.a. age-related macular degeneration - AMD). Also, hospitals are not interested in treatment of either DR or DME patients within low valued JGP groups (like B84 - laser fotocoagulation ) as it is not economically attractive, so they have retained the treatment within the most highest valued groups like B16 and B17 - vitrectomy - which is mainly used for the highest severe DR and DME patients.
Taking into account current situation in outpatient clinics where there is a very limited patients’ access (long queues) to the specialist, that limits DR and DME early stage diagnosis also considering JGP system structure and valuation, all of these circumstances markedly prevents from proper DR and DME treatment and vision loss prevention in the discussed population.
Current direct costs of DME treatment in Poland are low, and there is a space for improvement, as indirect costs of not treating the DME, including social security costs due to the deterioration of vision amongst diabetes patients might significantly exceed the costs of the disease treatment. Also further analyses, especially calculating DME costs in a social security system perspective might be helpful in taking any decisions regarding changes in the current treatment possibilities within the JGP groups system.
On top of the pharmacoeconomical divagations, there is a need to start a national program of evaluation of prevalence and incidence of diabetes mellitus related diseases including Diabetic Retinopathy and Diabetic Macular Edema.
- Khan BU, Lam W-C.: Macular Edema in Diabetes. Available at: http://emedicine.medscape.com/article/1224138-overview#a6; Published February 29, 2016; [Accessed August 13, 2016]
- Rohit Varma, MD, MPH1; Neil M. Bressler (…); JAMA Ophthalmol. 2014;132(11):1334-1340. doi:10.1001/jamaophthalmol.2014.2854; Available at: http://archopht.jamanetwork.com/article.aspx?articleid=1895297; [Accessed August 13, 2016]
- Joanne WY Yau, Sophie L Rogers, Ryo Kawasaki. Global Prevalence and Major Risk Factors of Diabetic Retinopathy, Available at http://care.diabetesjournals.org/content/35/3/556; Published February 1, 2012; [Accessed August 13, 2016]
- Coscas G, Cuhna-Vaz J. Macluar edema a practical approach, Developments in Opthalmology, S.Karger AG, 2010, p:74
- Javadzadeh A. The effect of posterior subtenon methylprednisolone acetate in the refractory diabetic macular edema: a prospective nonrandomized interventional case series. BMC Ophthalmol. 2006; 15-19
- Varma R, Torres M, Pena F, et al. Prevalence of diabetic retinopathy in adult Latinos: the Los Angeles Latino eye study. Ophthalmology 2004; 1298-1306
- West SK, Klein R, Rodriguez J, et al. Diabetes and diabetic retinopathy in a Mexican-American population: Proyecto VER. Diabetes Care 2001;1204-1209;
- Based on the NFZ data. Available at: http://nfz.gov.pl/nfz-blizej-pacjenta/cukrzyca/; Accessed: August 20, 2016
- Joanne WY Yau, Sophie L Rogers, Ryo Kawasaki. Global Prevalence and Major Risk Factors of Diabetic Retinopathy, Available at http://care.diabetesjournals.org/content/35/3/556; Published February 1, 2012; [Accessed August 13, 2016]
- Authors study, based on the: Statystyka JGP; Available at: http://www.nfz.gov.pl/zarzadzenia-prezesa/zarzadzenia-prezesa-nfz/zarzadzenie-nr-712016dsoz,6514.html and http://www.nfz.gov.pl/zarzadzenia-prezesa/zarzadzenia-prezesa-nfz/zarzadzenie-nr-892013dsoz,5855.html; [Accessed: August 19, 2016]
- Authors study, based on the: Statystyka JGP; Available at: https://prog.nfz.gov.pl/app-jgp/KatalogJGP.aspx; [Accessed: August 19, 2016]
- Authors study, based on the: Statystyka JGP; Available at: http://www.nfz.gov.pl/zarzadzenia-prezesa/zarzadzenia-prezesa-nfz/zarzadzenie-nr-712016dsoz,6514.html and http://www.nfz.gov.pl/zarzadzenia-prezesa/zarzadzenia-prezesa-nfz/zarzadzenie-nr-892013dsoz,5855.html; [Accessed: August 19, 2016]
- Authors study, based on the: Coscas G, Cuhna-Vaz J. Macluar edema a practical approach, Developments in Opthalmology, S.Karger AG, 2010, p:74; Javadzadeh A. The effect of posterior subtenon methylprednisolone acetate in the refractory diabetic macular edema: a prospective nonrandomized interventional case series. BMC Ophthalmol. 2006; 15-19; Varma R, Torres M, Pena F, et al. Prevalence of diabetic retinopathy in adult Latinos: the Los Angeles Latino eye study. Ophthalmology 2004; 1298-1306; West SK, Klein R, Rodriguez J, et al. Diabetes and diabetic retinopathy in a Mexican-American population: Proyecto VER. Diabetes Care 2001;1204-1209
- Authors study based on: Coscas G, Cuhna-Vaz J. Macluar edema a practical approach, Developments in Opthalmology, S.Karger AG, 2010, p:74; Javadzadeh A. The effect of posterior subtenon methylprednisolone acetate in the refractory diabetic macular edema: a prospective nonrandomized interventional case series. BMC Ophthalmol. 2006; 15-19
- Authors study, based on the: Statystyka JGP; Available at: https://prog.nfz.gov.pl/app-jgp/KatalogJGP.aspx; Accessed: August 20, 2016.
- Based on the NFZ data; Available at: http://nfz.gov.pl/nfz-blizej-pacjenta/cukrzyca/; Accessed: August 20, 2016
- Joanne WY Yau, Sophie L Rogers, Ryo Kawasaki. Global Prevalence and Major Risk Factors of Diabetic Retinopathy, Available at http://care.diabetesjournals.org/content/35/3/556; Published February 1, 2012; [Accessed August 13, 2016]
- Based on own study, DME calculator DME Hospitalisations = DR Hospitalisations *((82%*38%) + (18%*71%))
-
Authors study, based on the: Statystyka JGP; Available at: https://prog.nfz.gov.pl/app-jgp/KatalogJGP.aspx; [Accessed: August 20, 2016]
-
Authors study, based on the: Statystyka JGP; Available at: https://prog.nfz.gov.pl/app-jgp/KatalogJGP.aspx; [Accessed: August 20, 2016]